Medicaid Disenrollment Leading to UninsuranceMedicaid Disenrollment Leading to Uninsurance A recent study by the Harvard TH Chan School of Public Health has revealed that a significant number of Americans have lost Medicaid coverage during the “Medicaid unwinding” process. The study surveyed adults in four states who had Medicaid insurance as of March 2020 and found that: * 12.5% of respondents reported losing Medicaid coverage by fall 2023. * 48% of those who disenrolled were uninsured at the time of the survey. * Younger individuals, those living in rural areas, and women were more likely to become uninsured. Consequences of Medicaid Disenrollment The study also highlighted the negative consequences of Medicaid disenrollment on access to healthcare: * Those who lost coverage reported more cost-related delays in care, missed medication doses, and difficulty affording care. * They were also less likely to have had an annual checkup compared to those who maintained coverage. Policy Implications The study’s findings emphasize the need for policies to mitigate the negative effects of Medicaid coverage disruptions. Researchers suggest that policymakers consider the following: * Expanding Medicaid eligibility and simplifying enrollment processes. * Improving outreach and assistance to help eligible individuals retain coverage. * Establishing policies that allow individuals to maintain coverage during periods of income fluctuations or other life changes. The study reinforces the importance of ensuring access to affordable healthcare for all Americans. By addressing the challenges associated with Medicaid unwinding, policymakers can help reduce coverage gaps and protect the health and well-being of vulnerable populations.
A study from the Harvard TH Chan School of Public Health found that one in eight respondents who had Medicaid insurance as of March 2020 reported they would no longer have Medicaid coverage by the end of 2023. Nearly half of these respondents indicated that they were currently uninsured.
The researchers conducted the study from September to November 2023, about six months after the start of “Medicaid unwinding,” the process by which states re-verified the eligibility of Medicaid enrollees after the expiration of COVID-19-era coverage protections .
We know from government statistics that of the more than 90 million people whose health insurance was at risk due to the phaseout of Medicaid, more than 23 million have been dropped from the program. But those statistics don’t tell us what happened to those people or why they lost coverage. Our study is one of the first to help answer those outstanding questions, using completely new data from an original multi-state survey.”
Adrianna McIntyre, Assistant Professor of Health Policy and Politics, lead author
The research will be published on June 29 in JAMA Health Forum.
The researchers surveyed 2,210 adults ages 19 to 64 in those four states whose 2022 incomes were at or below 138% of the federal poverty level. Participants were asked whether they and/or their dependents had been enrolled in Medicaid at any time since March 2020, when states suspended Medicaid disenrollment as part of the COVID-19 federal public health emergency. They were also asked about their current health insurance and their ability to access care, as well as their demographics.
Most survey respondents (71%) reported that they and/or a dependent were enrolled in Medicaid at some point since March 2020. Of adult respondents who had Medicaid, 12.5% reported disenrolling by fall 2023. adult disenrollment levels varied: 16% in Arkansas, 15% in Texas, 8% in Louisiana, and 7% in Kentucky. Of those who had disenrolled, 52% had found another source of insurance, although a significant portion of these respondents reported coverage gaps. The remaining 48% of those deregistered indicated that they were not insured. Disenrollment was significantly higher among those who were younger, lived and/or worked in rural areas, and women were more likely than men to become uninsured. The reported disenrollment rate was much lower on average for dependent children (5.4%).
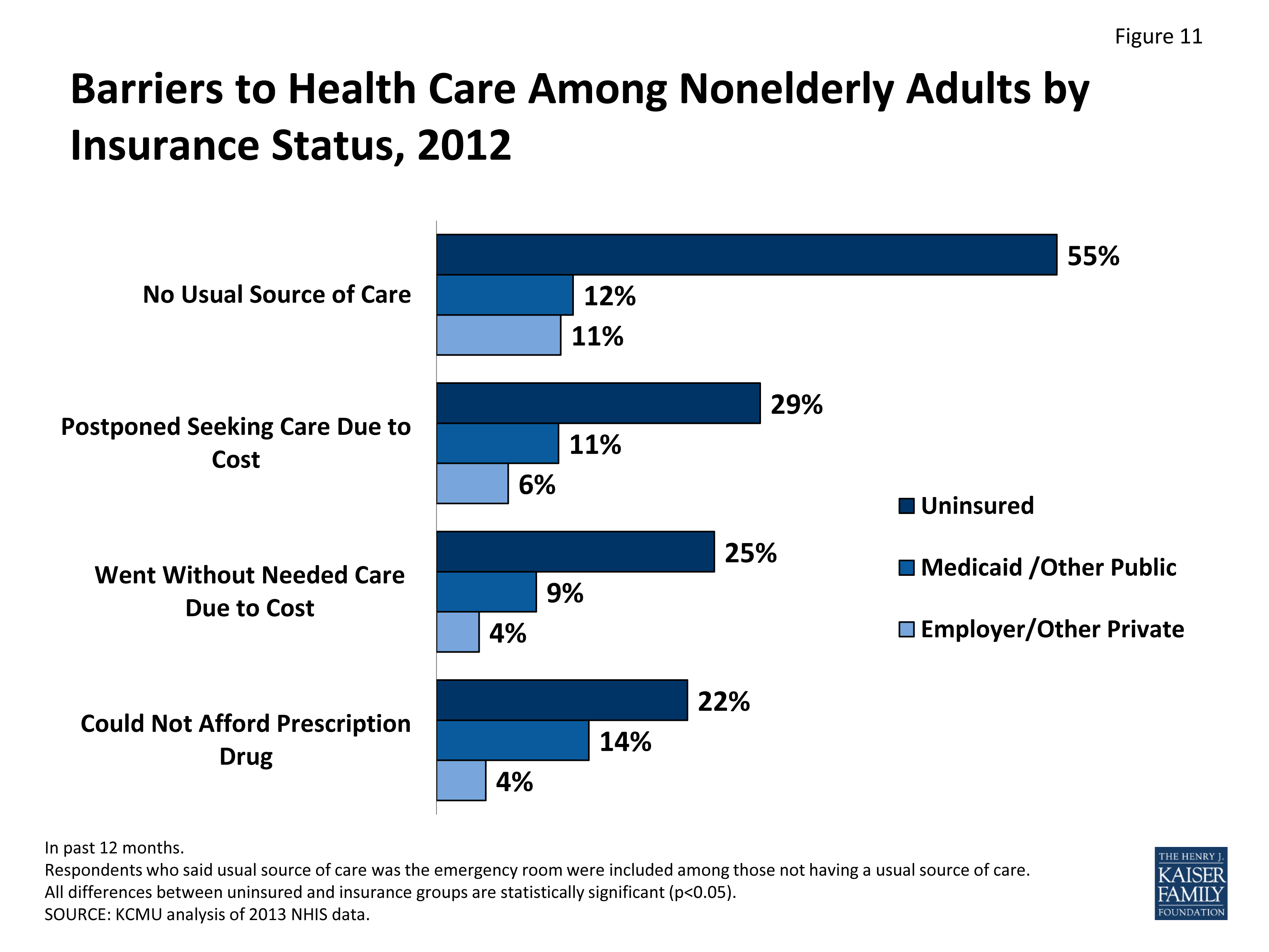
The study also found that those who were disenrolled had significantly worse access to health care than those who did not lose their Medicaid coverage. Those who disenrolled reported more cost-related delays in care (51% vs. 27%) and delays or missed doses of medications (45% vs. 27%); said care was less affordable than the previous year (47% vs. 22%); and have not had an annual check-up in the past year (57% versus 34%).
“Previous research has linked even brief coverage gaps to care disruptions and negative health outcomes,” McIntyre said. “Our findings suggest that policymakers at the state and federal levels should pursue policies to mitigate negative outcomes associated with coverage disruptions — not only during Medicaid phaseout, but also in the years ahead, as issues related to eligibility reassessment and coverage continuity will continue to be relevant in Medicaid.”
The researchers noted that the study’s findings are limited in their generalizability for a number of reasons. For example, the sample was limited to residents of four states who reported lower incomes, and there were significant differences in the states’ approaches to de-stressing.
Benjamin Sommers, Gabriella Aboulafia, Jessica Phelan, E. John Orav, Arnold Epstein and Jose Figueroa, all from Harvard Chan’s Department of Health Policy and Management, were co-authors.
The research received funding from the Commonwealth Fund and the Episcopal Health Foundation.
Source:
Harvard TH Chan School of Public Health
Magazine reference:
McIntyre, A., and all. (2024). Changes in coverage and access during the phaseout of Medicaid. JAMA Health Forum. doi.org/10.1001/jamahealthforum.2024.2193.